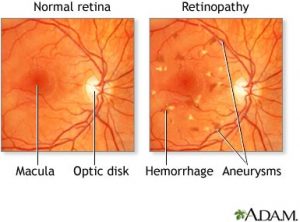
 High blood-sugar levels from diabetes can damage blood vessels in your retina, the layer of nerve tissue at the back of your eye. This damage is called diabetic retinopathy. Early diagnosis and treatment can prevent vision loss, and it’s important to maintain control of your blood sugar if you have diabetes.
High blood-sugar levels from diabetes can damage blood vessels in your retina, the layer of nerve tissue at the back of your eye. This damage is called diabetic retinopathy. Early diagnosis and treatment can prevent vision loss, and it’s important to maintain control of your blood sugar if you have diabetes.
What are the risk factors for diabetic retinopathy?
- You have type 1 diabetes
- You have type 2 diabetes
- You do not follow a strict diet
- You do not control your blood sugar levels
Reducing your risk
To reduce your risk or manage the disease, everyone with type 2 diabetes must be seen at least yearly by an ophthalmologist, Eye M.D., from the time of diabetes diagnosis. If you have been diagnosed with type 1 diabetes, you should see an ophthalmologist yearly beginning five years after the time of diabetes diagnosis.
Maintaining strict control of your blood sugar and following a strict diet are essential to preventing diabetic retinopathy in patients with diabetes.
Regular medical eye exams can help prevent unnecessary vision loss. The American Academy of Ophthalmology now recommends that adults with no signs or risk factors for eye disease get a baseline eye disease screening at age 40—the time when early signs of disease and changes in vision may start to occur. Based on the results of the initial screening, an Eye M.D. will prescribe the necessary intervals for follow-up exams.
Symptoms and Diagnosis
Often there are no symptoms in the early stages of diabetic retinopathy. Don’t wait for symptoms to have a comprehensive eye exam.
If you suddenly see a few specks or spots floating in your vision, this may indicate proliferative diabetic retinopathy, the growth of abnormal new blood vessels on your retina and optic nerve.
Blurred vision may occur when the macula – the small area at the center of the retina – swells from fluid leaking from retinal blood vessels. Rapid changes in blood sugar can cause temporary blurring of vision in both eyes even if retinopathy is not present.
You should have your eyes checked promptly if you experience changes in your vision that last more than a few days and are not associated with a change in blood sugar.
A medical eye examination is the best way to detect changes inside your eye. An ophthalmologist, Eye M.D., can often diagnose and treat serious retinopathy before you are aware of any vision problems. The doctor dilates your pupil and looks inside of the eye with special instruments.
If your Eye M.D. finds diabetic retinopathy, he or she may order color photographs of the retina. Your doctor may also order a special test called fluorescein angiography to find out if you need treatment. In this test, a dye is injected into your arm and photos of your eye are taken to detect where fluid is leaking.
People with diabetes should schedule examinations at least once a year. More frequent medical exams may be necessary after a diagnosis of diabetic retinopathy.
If you have diabetes and you are 29 years old or younger, see an Eye M.D. within five years of your diagnosis. If you are 30 years old or older, see an Eye M.D. within a few months of your diagnosis.
Pregnant women with diabetes should schedule an appointment in the first trimester, because retinopathy can progress quickly during pregnancy.
Last reviewed and updated in February 2009,
by the American Academy of Ophthalmology.
Image shown on Google Health.
